Gingival sulcus of the tooth
April 05, 2023
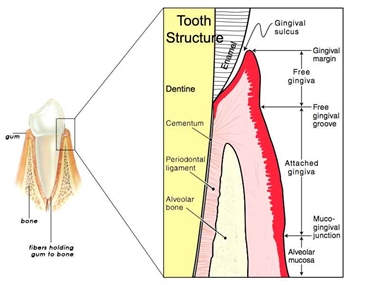
The tooth is supported by a complex of tissues called the periodontium. There are four tissues that makeup the periodontium - the alveolar bone, periodontal ligament, cementum and the gingiva. The alveolar bone is the underlying socket to in which the external surface of the tooth's roots (cementum) are positioned with the help of the periodontal ligament fibres. Additional support and blood supply is given by the gingival tissue that embraces the radicular (root portion) region of the tooth.
There are many areas in the human body where two structures lie adjacent to each other and yet there is a "potential space" between them. One such region is the gingival sulcus. This area is between the tooth and the attached portion of the gingiva. It is also known as the gingival crevice.
Anatomy of the dental sulcus
The gingival sulcus is a V-shaped groove. While the base is formed by the gingival fibres, the apex is formed by the free gingival margin. The depth of this groove till 3 mm is considered normal and healthy. This space is sufficient for the bristles of tooth to keep the area clean.
The lining of the gingival sulcus is called the sulcular epithelium. Flowing between this sulcular epithelium and the tooth surface is the gingival crevicular fluid (GCF). The GCF is a fluid whose flow rate is 0.2 microliters per hour. It's washing away mechanism keeps does not allow the accumulation of bacteria. However, the GCF also contains the substrates necessary for the bacteria to exert their pathogenic effect. Hence, this also makes it one of the promoters of inflammatory conditions of the gingiva.
Clinical examination of the gingival sulcus condition and depth
Clinical examination of the gingival sulcus is done in order to establish the health of the gingiva. During a routine dental examination, the dental surgeon uses a probe, which is a ruler-like thin hand-held device with measurements marked at certain intervals. If the depth of the gingival sulcus is less than 3 mm, then it is considered normal. However, in case this depth is more than 3 mm, then a pathologic inflammatory condition is suspected.
Pathology
Pathological conditions of the gingival sulcus begin when there is accumulation of debris, plaque and calculus in the gingival sulcus. This is usually a result of poor oral hygiene maintenance or the ill-effects of an existing systemic condition. The pathogenic microbes form a pathological pocket that extends beyond 3 mm of the sulcus depth. This leads to inflammation and recession of the gingiva. If untreated or ignored, the condition can worsen and affect the periodontal tissues. The resulting condition is called periodontitis.
When periodontitis occurs as a result of the abnormal depth of the gingival sulcus, it can have a direct effect on the attachment of the tooth to the underlying socket. This results in a mobile tooth and is subsequently at a risk of exfoliation.
Clinical signs and symptoms
When a patient presents with pain in the gums, bleeding of the gums while brushing, bad breath, swollen gums, then an abnormal depth of the gingival sulcus is suspected. In more severe cases, loose teeth, pain on chewing and loosening of an existing prosthesis may also take place. All these point towards an inflammatory condition that was triggered due to a gingival crevice getting pathologically inflamed.
Treatment options
The gingival sulcus needs a professional cleaning when it's depth increases more than 3 mm. This procedure is called scaling which is commonly done with ultrasonic devices that loosen up the accumulated plaque and calculus. In more severe cases a root planning is also done, wherein the depth of the professional cleaning extends till the level of the roots.
In some cases the exposure of the root surfaces due to gingival recession can lead to a cavity formation near the roots. In such cases, restorative treatment options are opted for. This includes removal of the carious portions with the dental drill, followed by restoring it with a biocompatible restorative dental cement.
A periodontist is a dental surgeon who is considered to be an expertise in severe cases of abnormal sulcular depth of the gingiva. They can carry out graft surgeries to re-establish the normal biological width. If needed, antibiotic chips may also be placed in these regions. Moreover, dental surgeons are now also trained to perform periodontal surgeries with lasers, which results in faster haling of the tissues. Antibiotics and analgesics may also be prescribed to the patient in order to reduce the microbial load and pain.
Gingival sulcus is a thin but a highly significant anatomical feature of the dental complex that plays a key role in the tooth's defensive mechanisms.

