How do we know if apicoectomy has failed
November 21, 2021


Root canal treatments are one of the most common treatment procedures in dentistry. This procedure is carried out in cases of a deep infection of the tooth or traumatic events that cause an irreversible inflammation within the tooth. The procedure is done by removing the carious portions, cleaning and shaping the root canals from within and finally dressing it with a biocompatible material. A final restoration in the form of a crown may or may not be given depending on the extent of tooth structure lost.
Root canal treatments, in most cases, resolve any infection of the tooth and reinstates a healthy tissue structure surrounding the tooth. However, there are cases when even after a root canal treatment, the infection within the tooth does not resolve. This is usually found at the tip of the roots. On a radiograph, it can be seen as a circular blackish structure attached to the root's tip. A patient will usually complain of pain upon chewing and sensitivity around the treated tooth. Swelling of the adjacent gums is also apparent in many cases. In some other cases, a patient will have no symptoms at all, and upon routine check-up the dentist will inform them about a re-infection after a radiographic examination. Such cases of re-infection can be approached by either re-performing the root canal procedure or opting for an apicoectomy.
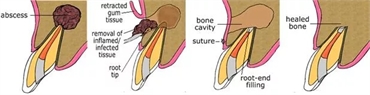
Apicoectomy is also known as root end surgery or root-end filling or retrograde root canal treatment. It is performed in cases of a failed root canal treatment. This procedure involves removal of 1-3 mm of the root's ends, followed by placement of a suitable biocompatible material in the space created. The removal of this minor portion of the root also leads to the removal of the associated infected substance.
An apicoectomy is done under a local anesthesia. Once the area is numbed, the gingiva near the roots of the affected tooth is incised and raised as a flap. This window-like structure allows the dental surgeon to visualise the end of the root. The end of the root along with the associated infected material is then removed. A suitable restorative material is placed to fill the void created. The flap is sutured back, which is removed after one or two weeks.
The patient is kept on a regular follow-up to evaluate the status of the tooth and its surrounding structures. Apicoectomy enjoys a success rate that is well over 90%. However, certain factors may lead to failure of the procedure. A patient can continue of persistent pain and swelling in the tooth that went through the apicoectomy procedure. The radiographic evaluation can continue to show the presence of infection. This is when an apicoectomy is considered a failure.
There are many reasons for an apicoectomy to fail. Firstly, the location of the tooth of concern is often challenging. Teeth that are placed behind are difficult to access. To raise a flap and remove a minor portion of the tip of the root poses even more challenges. These hurdles are now overcome by the help of microendodontic equipment which can help in better visibility. However, not every dental setting have these equipment.
Another reason of failure of apicoectomy is improper healing after the surgery. This is often associated with patients who have a habit of smoking, and thus, the tooth takes longer than normal time to heal.
Apicoectomy in lower back teeth have an added risk of nerve damage. Many important nerves of the face pass near the roots of these teeth. Upon incising and raising a flap, there is a chance that the dental surgeon damages a nerve in the process.
Apicoectomy in the upper back teeth are very close to the maxillary sinus. A perforation in the sinus is a major risk factor and can warrant further surgical procedures.
Reinfection may occur if the root cavity is not cleaned properly. Before the placement of a biomaterial, the cavity is cleansed through irrigants. If not done properly, the infective microbes left behind can thrive and continue to cause trouble.
A microleakage can occur if the biomaterial is not compressed properly against the root. A gap between the material and the root can welcome microbes in that region, leading to reinfection. This is often seen in cases where the material of choice is a composite resin. Composite resin requires a dry environment for better setting. The presence of moisture created by saliva can create a weak bond of the material with the tooth's root and can thus result in failure of the procedure. Mineral Trioxide Aggregate, amalgam, and modified versions of Zinc Oxide Eugenol can serve as better alternatives.
A failure of apicoectomy does not necessarily mean that the tooth needs to be removed. Since bone growth around the tooth after apicoectomy can take several months, performing an apicoectomy again can also be a viable alternative. However, in such cases apicoectomy needs to be coupled with curettage to remove the necrotic material and bone grafting techniques to accelerate healing. An extraction should only be done in teeth with hopeless prognosis wherein there is root resorption and development of soft tissue lesions.
Apicoectomy is a successful procedure and can help in preserving the natural tooth for longer periods. Modern advances have made it possible to perform apicoectomy with much ease and thus chances of it failing have reduced drastically. A failed apicoectomy can be due to many reasons. But even after that, the goal is to preserve the tooth as long as possible.

